Difference between revisions of "Bosy-Westphal 2009 Br J Nutr"
| Line 11: | Line 11: | ||
== From BMI to BME == | == From BMI to BME == | ||
''Work in progress'' by [[Gnaiger E]] 2020-02- | ''Work in progress'' by [[Gnaiger E]] 2020-02-09 linked to a preprint in preparation on [[body mass excess |'''BME''']] and [[:Category:BME and mitObesity |'''mitObesity''']]. | ||
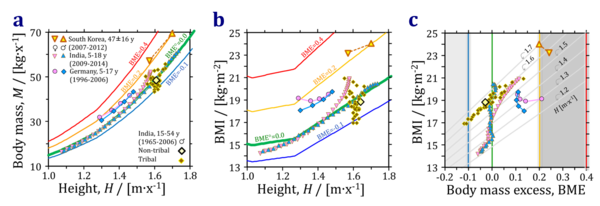
[[File:MfH-BMIfH-BMIfBME Asia.png|left|600px|thumb|'''Figure 1''': Body mass ('''a'''), and body mass index, BMI ('''b''') as a function of height. Data from the [[Indian Academy of Pediatrics Growth Charts Committee 2015 Indian Pediatr]], Hood et al (2019), and Bosy-Westphal et al (2009). South Korean women have a lower BMI than men, but are more displaced from the BME=0.2 cutoff line. ('''c''') BMI as a function of body mass excess, BME. At any constant height, the BMI increases linearly with BME (grey lines), but at constant BME the BMI increases as a function of height, from 15 kg·m<sup>-2</sup> at 1.2 m to 20 kg·m<sup>-2</sup> at 1.7 m.]] | [[File:MfH-BMIfH-BMIfBME Asia.png|left|600px|thumb|'''Figure 1''': Body mass ('''a'''), and body mass index, BMI ('''b''') as a function of height. Data from the [[Indian Academy of Pediatrics Growth Charts Committee 2015 Indian Pediatr]], Hood et al (2019), and Bosy-Westphal et al (2009). South Korean women have a lower BMI than men, but are more displaced from the BME=0.2 cutoff line. ('''c''') BMI as a function of body mass excess, BME. At any constant height, the BMI increases linearly with BME (grey lines), but at constant BME the BMI increases as a function of height, from 15 kg·m<sup>-2</sup> at 1.2 m to 20 kg·m<sup>-2</sup> at 1.7 m.]] | ||
{{References: BME and body fat}} | |||
{{References: BME and height}} | {{References: BME and height}} | ||
[[Category:BME and mitObesity]] | [[Category:BME and mitObesity]] | ||
Revision as of 18:16, 9 February 2020
| Bosy-Westphal A, Plachta-Danielzik S, Dörhöfer RP, Müller MJ (2009) Short stature and obesity: positive association in adults but inverse association in children and adolescents. Br J Nutr 102:453-61. |
Bosy-Westphal A, Plachta-Danielzik S, Doerhoefer RP, Mueller MJ (2009) Br J Nutr
Abstract: Shorter than average adults are at a higher risk for obesity and are also more susceptible to diabetes and CVD, independent of BMI. In contrast, taller children have a higher risk of obesity. We hypothesised that short stature is related to adverse body composition and that the association between stature and obesity differs between generations. In a cross-sectional German database of 213 804 adults and 12 411 children and adolescents, the prevalence of overweight and obesity was compared between percentiles of height. The association between stature and percentage of fat mass (%FM), lean BMI (LBMI; kg/m2) or waist:hip ratio (in children only) was analysed within BMI groups. In adults, the prevalence of BMI >30 kg/m2 gradually increased with decreasing percentile of height whereas in children and adolescents, a positive association between height and weight status was observed. Short-stature women and girls had a 0.8-3.2 % lower %FM than tall subjects (P < 0.05), whereas no trend for %FM was observed in males. When compared with tall subjects, LBMI was 0.2-0.6 kg/m2 lower in short-stature men, as well as obese women (P < 0.05). There was a non-significant trend for a lower LBMI and a higher waist:hip ratio in shorter children. In conclusion, short stature is associated with an increased risk of obesity in adults. Cardiometabolic risk in short stature is not explained by an adverse body composition.
• Bioblast editor: Gnaiger E
From BMI to BME
Work in progress by Gnaiger E 2020-02-09 linked to a preprint in preparation on BME and mitObesity.
Publications: BME and body fat
| Reference | |
|---|---|
| Bosy-Westphal 2009 Br J Nutr | Bosy-Westphal A, Plachta-Danielzik S, Dörhöfer RP, Müller MJ (2009) Short stature and obesity: positive association in adults but inverse association in children and adolescents. Br J Nutr 102:453-61. |
| Chambers 2020 J Appl Physiol (1985) | Chambers TL, Burnett TR, Raue U, Lee GA, Finch WH, Graham BM, Trappe TA, Trappe S (2020) Skeletal muscle size, function, and adiposity with lifelong aerobic exercise. J Appl Physiol (1985) 128:368–78. |
| Deurenberg 2001 Eur J Clin Nutr | Deurenberg P, Andreoli A, Borg P, Kukkonen-Harjula K, de Lorenzo A, van Marken Lichtenbelt WD, Testolin G, Vigano R, Vollaard N (2001) The validity of predicted body fat percentage from body mass index and from impedance in samples of five European populations. Eur J Clin Nutr 55:973-9. |
| Gallagher 2000 Am J Clin Nutr | Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y (2000) Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr 72:694-701. |
| Meeuwsen 2010 Clin Nutr | Meeuwsen S, Horgan GW, Elia M (2010) The relationship between BMI and percent body fat, measured by bioelectrical impedance, in a large adult sample is curvilinear and influenced by age and sex. Clin Nutr 29:560-6. |
| Mialich 2014 Nutr Hosp | Mialich MS, Martinez EZ, Jordao JJ (2014) Application of body mass index adjusted for fat mass (BMIfat) obtained by bioelectrical impedance in adults. Nutr Hosp 30:417-24. |
| Mialich 2018 J Electr Bioimp | Mialich MS, Silva BR, Jordao AA (2018) Cutoff points of BMI for classification of nutritional status using bioelectrical impedance analysis. J Electr Bioimp 9:24-30. |
| Misra 2019 J Postgrad Med | Misra P, Singh AK, Archana S, Lohiya A, Kant S (2019) Relationship between body mass index and percentage of body fat, estimated by bio-electrical impedance among adult females in a rural community of North India: A cross-sectional study. J Postgrad Med 65:134-40. |
| National Academies of Sciences, Engineering, and Medicine 2023 BMI and beyond | National Academies of Sciences, Engineering, and Medicine (2023) BMI and beyond: Considering context in measuring obesity and its applications: Proceedings of a workshop—in brief. The National Academies Press, Washington, DC. https://doi.org/10.17226/27185 |
| National Academies of Sciences, Engineering, and Medicine 2024 Body composition and obesity | National Academies of Sciences, Engineering, and Medicine (2024) Exploring the science on measures of body composition, body fat distribution, and obesity. National Academies Press, Washington, DC https://doi.org/10.17226/27461. |
| Romero-Corral 2008 Int J Obes (Lond) | Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, Allison TG, Batsis JA, Sert-Kuniyoshi FH, Lopez-Jimenez F (2008) Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond) 32:959-66. |
| Wollner 2017 J Public Health Res | Wollner M, Paulo Roberto BB, Alysson Roncally SC, Jurandir N, Edil LS (2017) Accuracy of the WHO's body mass index cut-off points to measure gender- and age-specific obesity in middle-aged adults living in the city of Rio de Janeiro, Brazil. J Public Health Res 6:904. |
Publications: BME and height
| Reference | |
|---|---|
| Bosy-Westphal 2009 Br J Nutr | Bosy-Westphal A, Plachta-Danielzik S, Dörhöfer RP, Müller MJ (2009) Short stature and obesity: positive association in adults but inverse association in children and adolescents. Br J Nutr 102:453-61. |
| De Onis 2007 Bull World Health Organization | de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J (2007) Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organization 85:660-7. |
| Gnaiger 2019 MiP2019 | OXPHOS capacity in human muscle tissue and body mass excess – the MitoEAGLE mission towards an integrative database (Version 6; 2020-01-12). |
| Hood 2019 Nutr Diabetes | Hood K, Ashcraft J, Watts K, Hong S, Choi W, Heymsfield SB, Gautam RK, Thomas D (2019) Allometric scaling of weight to height and resulting body mass index thresholds in two Asian populations. Nutr Diabetes 9:2. doi: 10.1038/s41387-018-0068-3. |
| Indian Academy of Pediatrics Growth Charts Committee 2015 Indian Pediatr | Indian Academy of Pediatrics Growth Charts Committee, Khadilkar V, Yadav S, Agrawal KK, Tamboli S, Banerjee M, Cherian A, Goyal JP, Khadilkar A, Kumaravel V, Mohan V, Narayanappa D, Ray I, Yewale V (2015) Revised IAP growth charts for height, weight and body mass index for 5- to 18-year-old Indian children. Indian Pediatr 52:47-55. |
| Zucker 1962 Committee on Biological Handbooks, Fed Amer Soc Exp Biol | Zucker TF (1962) Regression of standing and sitting weights on body weight: man. In: Growth including reproduction and morphological development. Altman PL, Dittmer DS, eds: Committee on Biological Handbooks, Fed Amer Soc Exp Biol:336-7. |
Labels: MiParea: Exercise physiology;nutrition;life style
Pathology: Obesity
BMI, BME, Fat, Height

