From Bioblast
Description
In the healthy reference population (HRP), there is zero body fat excess, BFE, and the fraction of excess body fat in the HRP is expressed - by definition - relative to the reference body mass, M°, at any given height. Importantly, body fat excess, BFE, and body mass excess, BME, are linearly related, which is not the case for the body mass index, BMI.
Abbreviation: BFE
Reference: Body mass excess
Events on mitObesity
- 2023 Jun 06: » Health Innovation Summit 2023 Vienna AT
| Healthy reference population | Body mass excess | BFE | BME cutoffs | BMI | H | M | VO2max | mitObesity drugs |
Communicated by Gnaiger Erich 2020-02-15 in: Catastrophe XXX XXX-mass Carol on BME and mitObesity of X-mass Carol
- The BMI is known to predict adiposity with limited accuracy, with poor correlations between BMI and percentage of body fat. Several attempts have been made to derive alternative anthropometric indexes. The body adiposity index (Bergman et al 2011), however, has been criticized as insufficiently accurate for clinical applications (Cerqueira et al 2018). Other attempts include a shift of BMI cutoffs for different ethnic groups, adjustment of parameters for ethnicity, sex and age in equations incorporating the BMI, or the BMI is replaced and height/waist circumference included in fitted algorithms (Gallagher et al 2000; Al-Gindan et al 2015; Woolcott, Bergman 2018).
- Body fat is conventionally expressed as BF%, which is the percentage of body fat mass relative to the total body mass. The body mass excess, BME, introduces a concept that does not consider whole-body fat percentage, BF%, as the relevant risk factor, but the excess body fat mass, MFE, is emphasized with respect to the healthy reference body mass and composition, empirically based on the allometry of the healthy reference population, HRP. Although M° is identical in females and males at any given height, the fraction of body fat is higher in females than males in the HRP, hence it is reasonable that BFE, - but not BF% - represents the common risk factor and indicator of obesity.
From BF% to body fat excess, BFE
- The BME is the excess body mass of an individual, ME = M-M° [kg/x], normalized for the reference body mass, M° [kg/x], BME = ME/M°. M° is calculated at a given height, H [m], from the allometric height-body mass relationship of the healthy reference population, HRP.
- BF% expresses body fat mass, MF [kg/x], as a percentage of total body mass (Gallagher et al 2000; Deurenberg et al 2001; Romero-Corral et al 2008; Bosy-Westphal et al 2009),
Eq. 1: BF% = 100*MF/M
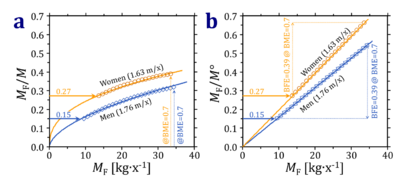
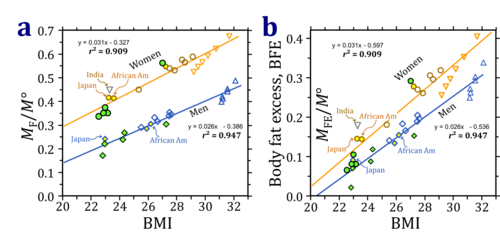
- MF increases due to accumulation of fat mass. Note that at any given height BF% or MF/M = BF%/100 increases non-linearly with attenuated slope as a function of MF (Fig. 1a). In contrast, normalization for M° - the reference body mass without excess fat mass - yields linear and proportional functions at constant height, since M° is a constant at any height (Fig. 1b).
- Figure 1: Model calculation on body fat mass, MF, normalized for (a) total body mass, M, and (b) reference body mass, M°. The relationship for women and men is shown at constant height of 1.63 and 1.76 m/x, with M° = of 51.2 and 63.8 kg/x. From BME = 0.0 to 0.7, M increases 1.7-fold to 87.2 and 108.8 kg per woman or man, respectively. The reference body fat mass fraction is estimated at 0.27 and 0.15 for women and men (horizontal full arrows), increasing to MF/M = 0.39 and 0.32, respectively (a: vertical dotted arrows). This covers the range of BME from 0.0 to 0.7 equally in women and men. Due to the 'weight-lifting effect', there is an excess lean mass, MLE, which is 0.75 times the excess fat mass, MLE = 0.75·MFE (Eq. 12). At the same BME of 0.7, the net increase or body fat excess, BFE = MFE/M°, is 0.39, identical in women and men (b: vertical dotted arrows).
Impact of experimental design
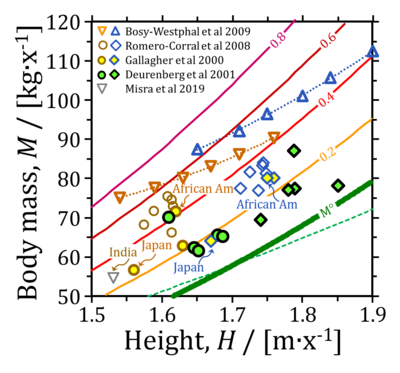
- Variation of body mass plotted as a function of height combines two determinants: (1) the allometric function in the healthy reference population, HRP, at zero body fat excess (M°), and (2) excess body mass (BME). The allometric exponent, HA, is A=2.89 in the range of heights covered in Fig. 2. An exponent of 2 is implied in the body mass index, BMI = M/H2. Allometric exponents in populations deviating from the HRP must be interpreted with care (Fig. 2; dotted lines for a study of females and malesof different heights), since the shift to overweight and obesity may affect subpopulations of different heights to different degrees (Bosy-Westphal et al 2009). Asian populations tend toward lower adult heights.
- Figure 2: Variation of body mass, M, as a function of height. M at identical BME is indicated by full lines (M° at BME=0.0; M at BME=0.2 to 0.8; equivalent to M=1.2M° to 1.8M°). The green dashed line indicates the allometric relation assumed in the definition of the BMI (exponent of 2, which is significantly lower then the exponent of 2.86 in the HRP). Dotted lines for females and males (data of Bosy-Westphal et al 2009). African American females are on average obese (BME>0.4), compared to African American males who are overweight (BME>0.2), whereas Japanese females and males are both close to the allometric overweight line (data of Gallagher et al 2000). Symbols not indicated by arrows are American or European Caucasian whites.
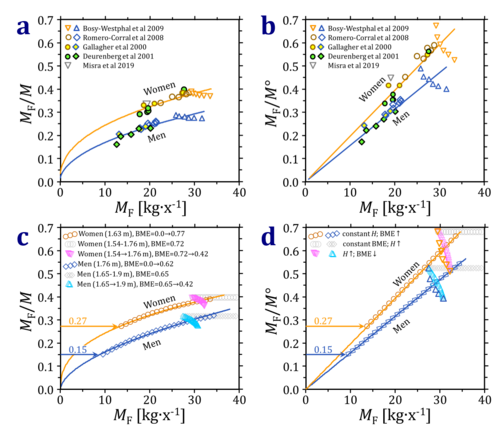
- Figure 3: Normalized body fat mass as a function total fat mass, MF. (a and b): Populations shown in Fig. 2. (c and d): Model calculations comparing strategies of selecting different groups. Body fat normalized for (a, c) total body mass, M, and (b, d) reference body mass, M°. Model 1: see Fig. 1 for increasing BME at constant height, H. Model 2: constant BME at increasing H. Model 3: from the study design of Bosy-Westphal et al 2009, when an increase in H is associated with a linear decrease in BME. The bold triangles depict the non-linear decrease in BME at the heights in the experimental data set. The excess lean mass, MLE, is assumed to be 0.8 times the exccess fat mass, MFE. See text for further explanations of the model calculations.
- As expected, the relationship between normalized fat mass and total fat mass is complicated in real data (Fig. 3a and 3b) compared to the simple model of constant height (Fig. 1). In agreement with the model in Fig. 1, however, normalization of body fat for the reference body mass, M°, yields a steeper slope and hence higher sensitivity (Fig. 3a and 3b).
- Taken together, two strategies are suggested by the above analyses for presenting the relative body fat excess, BFE: (1) normalization by the reference body mass, M°, and (2) subtraction of the reference body fat mass, MF-MF° (Fig. 1b). These two steps improve the relation between BFE and BMI (Fig. 4).
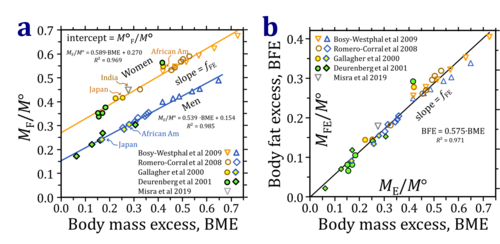
- Figure 4: Body fat mass correlated with BMI. (a) Total body fat mass, MF/M°, and (b) body fat excess, BFE = (MF-MF°)/M°. Asian populations tend to have higher fat mass at the same BMI, although there is a similarly large variability within Caucasian populations. Women have a higher relative fat mass at the same BMI compared to men. This difference is still apparent in the BFE. See Fig. 2 and 3 for further explanation of symbols.
- The purported differences between Asian and non-Asien populations is based on BMI (Fig. 4), ignoring the effect of height on BMI. In contrast, BME provides a unifying concept for ethnic groups of different evolutionary backgroud, with differences in body height as a key to normalize for appropriate reference body mass, M° (Fig. 5). Althoug M° at any given height is identical in women and men, a well defined difference exists in the reference body fat fraction between women and men, independent of height and evolutionary background of the populations covered in the original publications (Fig. 5a). Thus the large scatter implicated in using the BMI as an indicator of obesity (Fig. 4) is significantly reduced on the basis of the BME concept related to the healthy reference population. Body fat excess, BFE, is linearly related to body mass excess, BME (Fig. 5).
- Figure 5: Body mass excess, BME, as an indicator of (a) total body fat mass, MF/M°, and (b) body fat excess, BFE = (MF-MF°)/M° (Eq. 5b). R2 is 0.969 and 0.985 for women and men, respectively. The intercept at BME=0 is the relative body fat mass of the healthy reference population. This is 0.27 for women and 0.15 for men. The linear slopes are not significantly different in women and men, at 0.59 and 0.54, respectively (Eq. 9). The average slope, fFE = BFE/BME (Eq. 9) equals 0.57, which implies that 57 % of the increase in body mass is due to a gain of fat mass, and 43 % of the excess body mass is due to a gain of lean body mass (Eq. 11). The MLE/MFE ratio is 0.75 (Eq. 12). Data were calculated from tabulated values in the original references, including European and American Caucasian populations, African Americans, Japanese and Asien Indian populations as indicated.
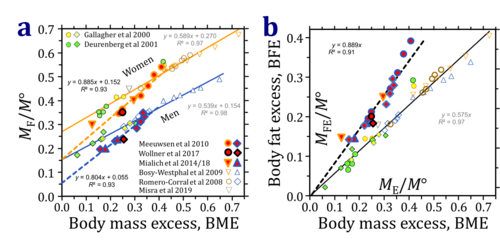
- For generalization, a detailed forcus is required on the different methods used for measurement of body fat. The data of Gallagher et al (2000) and Deurenberg et al (2001) are based on dual-energy X-ray absorptiometry (DXA). Romero-Corral et al (2008) and Bosy-Westphal et al (2009) describe in detail their method with body impedance analysis (see also Misra et al 2019). These studies use highly controlled samples with well-defined exclusion criteria. This is not the case for the self-selected sample used in the analyses of Meeuwsen et al (2010), and for the study of Mialich et al (2018), which included students, employees, patients and/or accompanying persons of a hospital (see also Mialich et al 2014). The latter studies were excluded in the analysis represented in Fig. 5, and are shown for comparison in Fig. 6. The further discussion is restricted to Fig. 5, and additional expert evaluation is required to resolve the discrepancies shown in Fig. 6.
- Figure 6: Body mass excess, BME, as an indicator of (a) total body fat mass, MF/M°, and (b) body fat excess, BFE = (MF-MF°)/M°, in two groups of data sources. Data of Fig. 5 are shown as small symbols. Added symbols (red filling) are based on bioelectrical impedance analysis, like the open symbols in Fig. 5 (and Fig. 6). The linear slopes in the two data sets are significantly different, but in each case identical in women and men, at 0.88 and 0.80, respectively, in the added data set, which includes ethnically mixed populations (UK: Meeuwsen et al 2010; Brazil: Wollner et al 2017; Mialich et al 2014, 2018).
Body fat in the healthy reference population
- The healthy reference population, HRP, is a population without excess body fat (no overweight) nor underweight (no ‘negative excess’ body fat) over the entire allometric range of height, H, and corresponding reference body mass, M°. The HRP has a body mass excess of zero, BME=0. By extrapolation of the relation between normalized body fat mass, MF/M°, and BME to the intercept at BME=0 (Fig. 5a), therefore, we obtain the fraction of body fat in the HRP, M°F/M°, which is higher in women (0.27) compared to men (0.15). Three resilient features are most remarkable in the linear (or very nearly linear) plots of MF/M° as a function of BME (Fig. 5a),
Eq. 2: MF/M° = slope·BME + intercept
- Whereas the allometric function of H/MA in the HRP (M=M°) is practically identical in females and males, the intercept M°F/M° is nearly twice in women than men (Fig. 5a).
- The slopes are practically identical in women and men (Fig. 5a). This provides a key rationale of the concept of body fat excess, BFE (Fig. 5b). Body mass excess, BME, constitutes a linearly proportional measure of BFE for women and men, over large ranges of height and a remarkable diversity of evolutionary backgrounds. However, no generalization to all ethnic populations is possible.
- The linear slope can be rationalized by a minimum model of BME related to accumulation of body fat. Note that the range of underweight with negative BME requires an entirely different analysis. For interpretation of Eq. 2, consider the total body mass as the sum of the reference body mass, M°, and excess body mass, ME,
Eq. 3: M ≝ M° + ME
- Excess body mass results from excess fat mass, MFE, and excess non-fat (lean) mass, MLE,
Eq. 4: ME = MFE + MLE
- It is useful to summarize some simple definitions of excess mass normalized for M°,
Eq. 5a Body mass excess: BME = ME/M° = M/M°-M°/M° Eq. 5b Body fat mass excess: BFE = MFE/M° = MF/M°-M°F/M° Eq. 5c Body lean mass excess: BLE = MLE/M° = ML/M°-M°L/M°
- Dividing Eq. 3 by M° and inserting definitions of Eq. 4 and Eq. 5,
Eq. 6: M/M° = 1 + BFE + BLE
- Solving for BFE and inserting Eq. 5a,
Eq. 7: BFE = BME - BLE
- M°F/M° is the intercept of Eq. 2, which can be expressed by inserting BFE from Eq. 5b in the simplified form (Fig. 5b),
Eq. 8: BFE = slope∙BME
- Therefore, the slope is the proportionality constant between BFE and BME. In other words, the slope is the fraction, fFE, of body fat excess contributing to total body mass excess,
Eq. 9: fFE = BFE/BME
- Since the slope is less than one, fFE<1, non-fat (lean) mass contributes to the total body mass excess. BLE (Eq. 5c) is due to the mechanical ‘weight-lifting’ effect: long-term adjustments to excess weight are known to induce heavier and larger (but not longer) bones, an increase in low-aerobic capacity muscle mass, and possibly other non-fat contributors to excess lean body mass, MLE. MLE includes increased bone mineral density, added bone mass and muscle mass (Iwaniec 2016 J Endocrinol).
- The linear slope (Eq. 7; Fig. 5) requires that BLE is a linear function of BME (compare Eq. 9),
Eq. 10: fLE = BLE/BME
- Substituting BLE = fLE∙BME in Eq. 7,
Eq. 11: BFE = (1-fLE)∙BME
- From Eq. 8 the slope is fFE=0.57 (Fig. 5b), and fFE = 1- fLE (Eq. 11); thus fLE=0.43. A slope fFE of 0.5 would suggest that BFE and BLE contribute equally to BME. fFE>0.5 indicates that BFE accounts for a higher contribution than BLE to BME. The excess lean mass due to the 'weight-lifting effect', MLE, is 0.75 times the excess fat mass, MLE = 0.75·MFE. The factor 0.75 is the MLE/MFE ratio (Fig. 1),
Eq. 12: MLE/MFE = (1/fFE)-1
- Body fat in the healthy reference population - a complementary route
- Eq. 12 is derived by beginning again: M is the sum of the reference mass at a given height, M°, and excess body mass, ME (Eq. 3). ME is accumulation of excess fat mass, MFE, accompanied by a gain of excess lean mass, MLE. Inserting ME ≝ MFE + MLE (Eq. 4) into Eq. 3,
Eq. 13: M = M° + MFE + MLE
- The fat mass, MF, is the sum of the reference fat mass and excess fat mass, MF ≝ M°F+MFE (Eq. 5b), hence
Eq. 14: MFE ≝ MF - M°F
- Inserting Eq. 14 into Eq. 13 yields body mass as the sum of the reference mass plus the total body fat mass minus the reference fat mass, plus the excess lean mass,
Eq. 15: M = M° + MF - M°F + MLE
- Normalization of Eq. 15 for M° and considering that the body mass excess is BME=M/M°-1 (Eq. 5a), BFE = (MF-M°F)/M° (Eq. 5b), and BLE = MLE/M° (Eq. 5c), yields Eq. 7 in the form of,
Eq. 16: BME = BFE + BLE
- By further normalization of Eq. 16 for BME, we obtain the summation of fFE = BFE/BME (Eq. 9) and fLE = BLE/BME (Eq. 10),
Eq. 17: 1 = fFE + fLE
- where fFE = 0.57 is the slope in Fig. 5b.
- To derive the MLE/MFE ratio (Eq. 12), which is equal to BLE/BFE (Eq. 5b and 5c), Eq. 16 is divided by BFE and rearranged,
Eq. 18: BLE/BFE = BME/BFE - 1
- Eq. 18 is equivalent to Eq. 12, since BME/BFE = 1/fFE (Eq. 9).
References: Body fat
- - >>>>>>> - Click on [Expand] or [Collapse] - >>>>>>>
| Reference | |
|---|---|
| Al-Gindan 2015 Br J Nutr | Al-Gindan YY, Hankey CR, Govan L, Gallagher D, Heymsfield SB, Lean ME (2015) Derivation and validation of simple anthropometric equations to predict adipose tissue mass and total fat mass with MRI as the reference method. Br J Nutr 114:1852-67. |
| Bergman 2011 Obesity (Silver Spring) | Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, Xiang AH, Watanabe RM (2011) A better index of body adiposity. Obesity (Silver Spring) 19:1083-9. |
| Bosy-Westphal 2009 Br J Nutr | Bosy-Westphal A, Plachta-Danielzik S, Dörhöfer RP, Müller MJ (2009) Short stature and obesity: positive association in adults but inverse association in children and adolescents. Br J Nutr 102:453-61. |
| Cerqueira 2018 Adv Nutr | Cerqueira MS, Santos CAD, Silva DAS, Amorim PRDS, Marins JCB, Franceschini SDCC (2018) Validity of the body adiposity index in predicting body fat in adults: a systematic review. Adv Nutr 9:617-24. |
| Chambers 2020 J Appl Physiol (1985) | Chambers TL, Burnett TR, Raue U, Lee GA, Finch WH, Graham BM, Trappe TA, Trappe S (2020) Skeletal muscle size, function, and adiposity with lifelong aerobic exercise. J Appl Physiol (1985) 128:368–78. |
| Da Silva 2017 Nutrition | da Silva BR, Mialich MS, de Paula FJA, Jordao AA (2017) Comparison of new adiposity indices for the prediction of body fat in hospitalized patients. Nutrition 42:99-105. |
| Deurenberg 2001 Eur J Clin Nutr | Deurenberg P, Andreoli A, Borg P, Kukkonen-Harjula K, de Lorenzo A, van Marken Lichtenbelt WD, Testolin G, Vigano R, Vollaard N (2001) The validity of predicted body fat percentage from body mass index and from impedance in samples of five European populations. Eur J Clin Nutr 55:973-9. |
| Gallagher 2000 Am J Clin Nutr | Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y (2000) Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr 72:694-701. |
| Heymsfield 2007 Am J Clin Nutr | Heymsfield SB, Gallagher D, Mayer L, Beetsch J, Pietrobelli A (2007) Scaling of human body composition to stature: new insights into body mass index. Am J Clin Nutr 86:82-91. |
| Hwaung 2020 Obes Rev | Hwaung P, Heo M, Kennedy S, Hong S, Thomas DM, Shepherd J, Heymsfield SB (2020) Optimum waist circumference-height indices for evaluating adult adiposity: An analytic review. Obes Rev 21(1):e12947. doi: 10.1111/obr.12947. |
| Keys 2014 Int J Epidemiol | Keys A, Fidanza F, Karvonen MJ, Kimura N, Taylor HL (2014) Indices of relative weight and obesity. Int J Epidemiol 43:655-65. |
| Kuper 2014 BMC Public Health | Kuper H, Taylor A, Krishna KV, Ben-Shlomo Y, Gupta R, Kulkarni B, Prabhakaran D, Davey Smith G, Wells J, Ebrahim S, Kinra S (2014) Is vulnerability to cardiometabolic disease in Indians mediated by abdominal adiposity or higher body adiposity. BMC Public Health 14:1239. |
| Meeuwsen 2010 Clin Nutr | Meeuwsen S, Horgan GW, Elia M (2010) The relationship between BMI and percent body fat, measured by bioelectrical impedance, in a large adult sample is curvilinear and influenced by age and sex. Clin Nutr 29:560-6. |
| Mendham 2020 Sci Rep | Mendham Amy E, Larsen Steen, George Cindy, Adams Kevin, Hauksson Jon, Olsson Tommy, Fortuin-de Smidt Melony C, Nono Nankam Pamela A, Hakim Olah, Goff Louise M, Pheiffer Carmen, Goedecke Julia H (2020) Exercise training results in depot-specific adaptations to adipose tissue mitochondrial function. Sci Rep 10:3785. |
| Mialich 2014 Nutr Hosp | Mialich MS, Martinez EZ, Jordao JJ (2014) Application of body mass index adjusted for fat mass (BMIfat) obtained by bioelectrical impedance in adults. Nutr Hosp 30:417-24. |
| Mialich 2018 J Electr Bioimp | Mialich MS, Silva BR, Jordao AA (2018) Cutoff points of BMI for classification of nutritional status using bioelectrical impedance analysis. J Electr Bioimp 9:24-30. |
| Misra 2019 J Postgrad Med | Misra P, Singh AK, Archana S, Lohiya A, Kant S (2019) Relationship between body mass index and percentage of body fat, estimated by bio-electrical impedance among adult females in a rural community of North India: A cross-sectional study. J Postgrad Med 65:134-40. |
| National Academies of Sciences, Engineering, and Medicine 2023 BMI and beyond | National Academies of Sciences, Engineering, and Medicine (2023) BMI and beyond: Considering context in measuring obesity and its applications: Proceedings of a workshop—in brief. The National Academies Press, Washington, DC. https://doi.org/10.17226/27185 |
| National Academies of Sciences, Engineering, and Medicine 2024 Body composition and obesity | National Academies of Sciences, Engineering, and Medicine (2024) Exploring the science on measures of body composition, body fat distribution, and obesity. National Academies Press, Washington, DC https://doi.org/10.17226/27461. |
| Nevill 2015 Nutr Diabetes | Nevill AM, Metsios GS (2015) The need to redefine age- and gender-specific overweight and obese body mass index cutoff points. Nutr Diabetes 5:e186. |
| Romero-Corral 2008 Int J Obes (Lond) | Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, Allison TG, Batsis JA, Sert-Kuniyoshi FH, Lopez-Jimenez F (2008) Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond) 32:959-66. |
| Thomas 2012 Nutr Res Rev | Thomas EL, Frost G, Taylor-Robinson SD, Bell JD (2012) Excess body fat in obese and normal-weight subjects. Nutr Res Rev 25:150–61. |
| Wells 2020 Lancet | Wells JC, Sawaya AL, Wibaek R, Mwangome M, Poullas MS, Yajnik CS, Demaio A (2020) The double burden of malnutrition: aetiological pathways and consequences for health. Lancet 395:75-88. |
| Wollner 2017 J Public Health Res | Wollner M, Paulo Roberto BB, Alysson Roncally SC, Jurandir N, Edil LS (2017) Accuracy of the WHO's body mass index cut-off points to measure gender- and age-specific obesity in middle-aged adults living in the city of Rio de Janeiro, Brazil. J Public Health Res 6:904. |
| Woolcott 2018 Sci Rep | Woolcott OO, Bergman RN (2018) Relative fat mass (RFM) as a new estimator of whole-body fat percentage ─ A cross-sectional study in American adult individuals. Sci Rep 8:10980. |
| Xiao 2019 Int J Hypertens | Xiao X, Wang W, Sa R, Qiu L, Liu F (2019) The investigation of sex differences in the effect of body mass index. Int J Hypertens 2019:1360328. |
Publications: BME and body fat
| Reference | |
|---|---|
| Bosy-Westphal 2009 Br J Nutr | Bosy-Westphal A, Plachta-Danielzik S, Dörhöfer RP, Müller MJ (2009) Short stature and obesity: positive association in adults but inverse association in children and adolescents. Br J Nutr 102:453-61. |
| Chambers 2020 J Appl Physiol (1985) | Chambers TL, Burnett TR, Raue U, Lee GA, Finch WH, Graham BM, Trappe TA, Trappe S (2020) Skeletal muscle size, function, and adiposity with lifelong aerobic exercise. J Appl Physiol (1985) 128:368–78. |
| Deurenberg 2001 Eur J Clin Nutr | Deurenberg P, Andreoli A, Borg P, Kukkonen-Harjula K, de Lorenzo A, van Marken Lichtenbelt WD, Testolin G, Vigano R, Vollaard N (2001) The validity of predicted body fat percentage from body mass index and from impedance in samples of five European populations. Eur J Clin Nutr 55:973-9. |
| Gallagher 2000 Am J Clin Nutr | Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y (2000) Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr 72:694-701. |
| Meeuwsen 2010 Clin Nutr | Meeuwsen S, Horgan GW, Elia M (2010) The relationship between BMI and percent body fat, measured by bioelectrical impedance, in a large adult sample is curvilinear and influenced by age and sex. Clin Nutr 29:560-6. |
| Mialich 2014 Nutr Hosp | Mialich MS, Martinez EZ, Jordao JJ (2014) Application of body mass index adjusted for fat mass (BMIfat) obtained by bioelectrical impedance in adults. Nutr Hosp 30:417-24. |
| Mialich 2018 J Electr Bioimp | Mialich MS, Silva BR, Jordao AA (2018) Cutoff points of BMI for classification of nutritional status using bioelectrical impedance analysis. J Electr Bioimp 9:24-30. |
| Misra 2019 J Postgrad Med | Misra P, Singh AK, Archana S, Lohiya A, Kant S (2019) Relationship between body mass index and percentage of body fat, estimated by bio-electrical impedance among adult females in a rural community of North India: A cross-sectional study. J Postgrad Med 65:134-40. |
| National Academies of Sciences, Engineering, and Medicine 2023 BMI and beyond | National Academies of Sciences, Engineering, and Medicine (2023) BMI and beyond: Considering context in measuring obesity and its applications: Proceedings of a workshop—in brief. The National Academies Press, Washington, DC. https://doi.org/10.17226/27185 |
| National Academies of Sciences, Engineering, and Medicine 2024 Body composition and obesity | National Academies of Sciences, Engineering, and Medicine (2024) Exploring the science on measures of body composition, body fat distribution, and obesity. National Academies Press, Washington, DC https://doi.org/10.17226/27461. |
| Romero-Corral 2008 Int J Obes (Lond) | Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, Allison TG, Batsis JA, Sert-Kuniyoshi FH, Lopez-Jimenez F (2008) Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond) 32:959-66. |
| Wollner 2017 J Public Health Res | Wollner M, Paulo Roberto BB, Alysson Roncally SC, Jurandir N, Edil LS (2017) Accuracy of the WHO's body mass index cut-off points to measure gender- and age-specific obesity in middle-aged adults living in the city of Rio de Janeiro, Brazil. J Public Health Res 6:904. |
MitoPedia: BME and mitObesity
» Body mass excess and mitObesity | BME and mitObesity news | Summary |
| Term | Abbreviation | Description |
|---|---|---|
| BME cutoff points | BME cutoff | Obesity is defined as a disease associated with an excess of body fat with respect to a healthy reference condition. Cutoff points for body mass excess, BME cutoff points, define the critical values for underweight (-0.1 and -0.2), overweight (0.2), and various degrees of obesity (0.4, 0.6, 0.8, and above). BME cutoffs are calibrated by crossover-points of BME with established BMI cutoffs. |
| Body fat excess | BFE | In the healthy reference population (HRP), there is zero body fat excess, BFE, and the fraction of excess body fat in the HRP is expressed - by definition - relative to the reference body mass, M°, at any given height. Importantly, body fat excess, BFE, and body mass excess, BME, are linearly related, which is not the case for the body mass index, BMI. |
| Body mass | m [kg]; M [kg·x-1] | The body mass M is the mass (kilogram [kg]) of an individual (object) [x] and is expressed in units [kg/x]. Whereas the body weight changes as a function of gravitational force (you are weightless at zero gravity; your floating weight in water is different from your weight in air), your mass is independent of gravitational force, and it is the same in air and water. |
| Body mass excess | BME | The body mass excess, BME, is an index of obesity and as such BME is a lifestyle metric. The BME is a measure of the extent to which your actual body mass, M [kg/x], deviates from M° [kg/x], which is the reference body mass [kg] per individual [x] without excess body fat in the healthy reference population, HRP. A balanced BME is BME° = 0.0 with a band width of -0.1 towards underweight and +0.2 towards overweight. The BME is linearly related to the body fat excess. |
| Body mass index | BMI | The body mass index, BMI, is the ratio of body mass to height squared (BMI=M·H-2), recommended by the WHO as a general indicator of underweight (BMI<18.5 kg·m-2), overweight (BMI>25 kg·m-2) and obesity (BMI>30 kg·m-2). Keys et al (1972; see 2014) emphasized that 'the prime criterion must be the relative independence of the index from height'. It is exactly the dependence of the BMI on height - from children to adults, women to men, Caucasians to Asians -, which requires adjustments of BMI-cutoff points. This deficiency is resolved by the body mass excess relative to the healthy reference population. |
| Comorbidity | Comorbidities are common in obesogenic lifestyle-induced early aging. These are preventable, non-communicable diseases with strong associations to obesity. In many studies, cause and effect in the sequence of onset of comorbidities remain elusive. Chronic degenerative diseases are commonly obesity-induced. The search for the link between obesity and the etiology of diverse preventable diseases lead to the hypothesis, that mitochondrial dysfunction is the common mechanism, summarized in the term 'mitObesity'. | |
| Healthy reference population | HRP | A healthy reference population, HRP, establishes the baseline for the relation between body mass and height in healthy people of zero underweight or overweight, providing a reference for evaluation of deviations towards underweight or overweight and obesity. The WHO Child Growth Standards (WHO-CGS) on height and body mass refer to healthy girls and boys from Brazil, Ghana, India, Norway, Oman and the USA. The Committee on Biological Handbooks compiled data on height and body mass of healthy males from infancy to old age (USA), published before emergence of the fast-food and soft-drink epidemic. Four allometric phases are distinguished with distinct allometric exponents. At heights above 1.26 m/x the allometric exponent is 2.9, equal in women and men, and significantly different from the exponent of 2.0 implicated in the body mass index, BMI [kg/m2]. |
| Height of humans | h [m]; H [m·x-1] | The height of humans, h, is given in SI units in meters [m]. Humans are countable objects, and the symbol and unit of the number of objects is N [x]. The average height of N objects is, H = h/N [m/x], where h is the heights of all N objects measured on top of each other. Therefore, the height per human has the unit [m·x-1] (compare body mass [kg·x-1]). Without further identifyer, H is considered as the standing height of a human, measured without shoes, hair ornaments and heavy outer garments. |
| Length | l [m] | Length l is an SI base quantity with SI base unit meter m. Quantities derived from length are area A [m2] and volume V [m3]. Length is an extensive quantity, increasing additively with the number of objects. The term 'height' h is used for length in cases of vertical position (see height of humans). Length of height per object, LUX [m·x-1] is length per unit-entity UX, in contrast to lentgth of a system, which may contain one or many entities, such as the length of a pipeline assembled from a number NX of individual pipes. Length is a quantity linked to direct sensory, practical experience, as reflected in terms related to length: long/short (height: tall/small). Terms such as 'long/short distance' are then used by analogy in the context of the more abstract quantity time (long/short duration). |
| MitObesity drugs | Bioactive mitObesity compounds are drugs and nutraceuticals with more or less reproducible beneficial effects in the treatment of diverse preventable degenerative diseases implicated in comorbidities linked to obesity, characterized by common mechanisms of action targeting mitochondria. | |
| Obesity | Obesity is a disease resulting from excessive accumulation of body fat. In common obesity (non-syndromic obesity) excessive body fat is due to an obesogenic lifestyle with lack of physical exercise ('couch') and caloric surplus of food consumption ('potato'), causing several comorbidities which are characterized as preventable non-communicable diseases. Persistent body fat excess associated with deficits of physical activity induces a weight-lifting effect on increasing muscle mass with decreasing mitochondrial capacity. Body fat excess, therefore, correlates with body mass excess up to a critical stage of obesogenic lifestyle-induced sarcopenia, when loss of muscle mass results in further deterioration of physical performance particularly at older age. | |
| VO2max | VO2max; VO2max/M | Maximum oxygen consumption, VO2max, is and index of cardiorespiratory fitness, measured by spiroergometry on human and animal organisms capable of controlled physical exercise performance on a treadmill or cycle ergometer. VO2max is the maximum respiration of an organism, expressed as the volume of O2 at STPD consumed per unit of time per individual object [mL.min-1.x-1]. If normalized per body mass of the individual object, M [kg.x-1], mass specific maximum oxygen consumption, VO2max/M, is expressed in units [mL.min-1.kg-1]. |
MitoPedia concepts:
MiP concept
Labels:
MitoPedia:BME